CTAD 2023 – Spotlight on recent advances in blood-based biomarkers for Alzheimer’s disease
By Dr. Nathalie Le Bastard, Fujirebio Europe
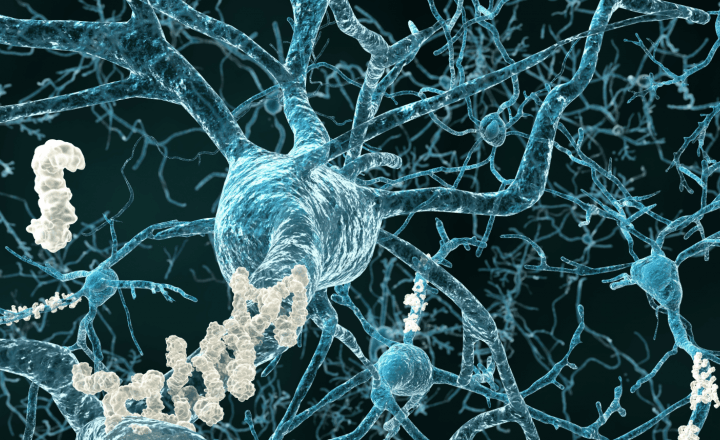
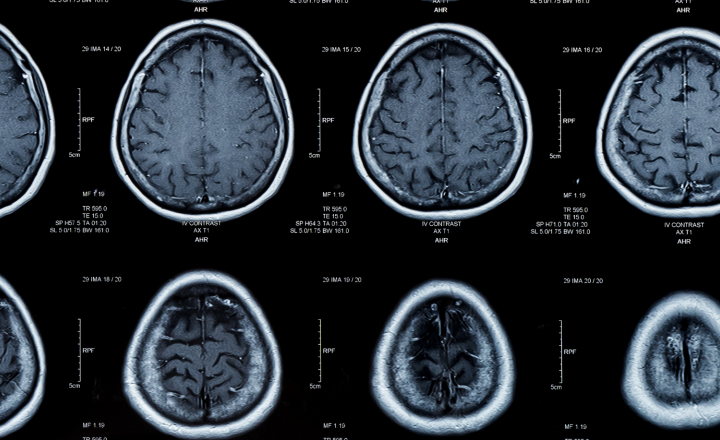
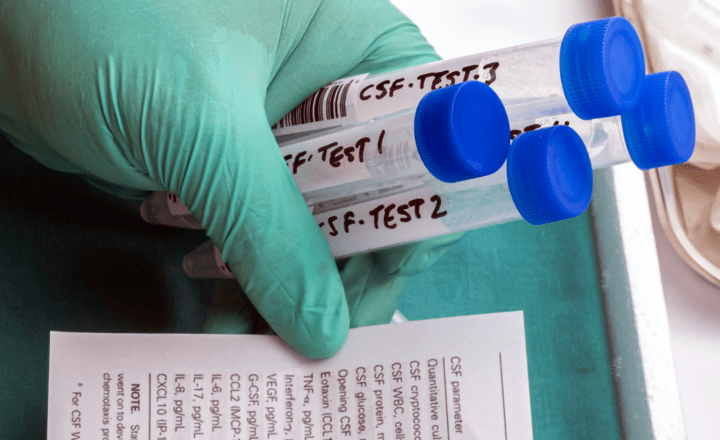
Both fluid and imaging biomarkers provide biological evidence for the underlying etiology of cognitive impairment. The core fluid biomarkers of Alzheimer’s disease (AD) pathology, i.e. Aβ1-42/1-40, tTau and pTau181 in cerebrospinal fluid (CSF), have long been identified and their clinical diagnostic performance established. In recent years, their implementation in clinical practice has been increasing due to the level of automation of the currently available tests and regulatory clearance in several regions around the world, e.g., Europe, United States and Japan.
However, with the advent of amyloid-targeting disease-modifying treatments for AD comes a great need for easier, less invasive, and more scalable tools to confirm the presence of amyloid (and perhaps also tau) pathology. The emergence of blood-based biomarkers, and sensitive immunoassays to detect these, are becoming a game-changer for the AD field, currently in a transition phase during which blood-based biomarkers are being integrated with “traditional” CSF and positron emission tomography (PET) biomarkers.1
It seems realistic to assume that certain plasma biomarker assays - currently only used in a research environment - could reach a high agreement with existing biomarker classifications or measurement tools, if used within a specific intended use setting. This is illustrated by the below examples presented during the latest Clinical Trials in Alzheimer’s Disease (CTAD) meeting.
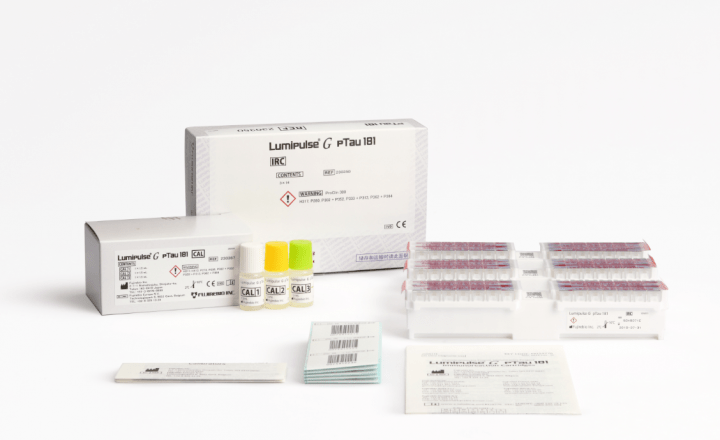
The work presented by Ashton et al.2 (LP048 – The Alzheimer’s Association Global Biomarker Standardization Consortium (GBSC) plasma phospho-tau Round Robin study – S138) reports the results from the largest head-to-head comparison to date including 26 different pTau assays. To estimate the clinical performance, a total of 40 individuals with suspected AD were evaluated and categorized in 25 AD and 15 non-AD cases according to their CSF biomarker profile and the matching plasma samples were measured with each of the participating assays. The discriminative accuracy (represented by the area under the curve (AUC)) as well as the mean fold change between the AD and non-AD group was generally higher for the plasma pTau217 assays. Some assays even achieved a perfect (100%) agreement with the CSF biomarker classification, despite the moderate correlation between CSF and plasma pTau which is most likely due to a complete loss of correlation in the AD group. The plasma pTau181 assays show a wider range in performance with the best performing pTau181 assay achieving an AUC of approximately 0.95, while another cannot distinguish between CSF biomarker positive and negative cases. Other results coming from the current study of significant importance are the strong correlations between the different pTau assays, contrary to the results obtained in similar studies for plasma amyloid in the past.3,4,5 In conclusion, the results of the current study tend to favor pTau217 as the blood-based biomarker of choice over any of the other pTau epitopes.
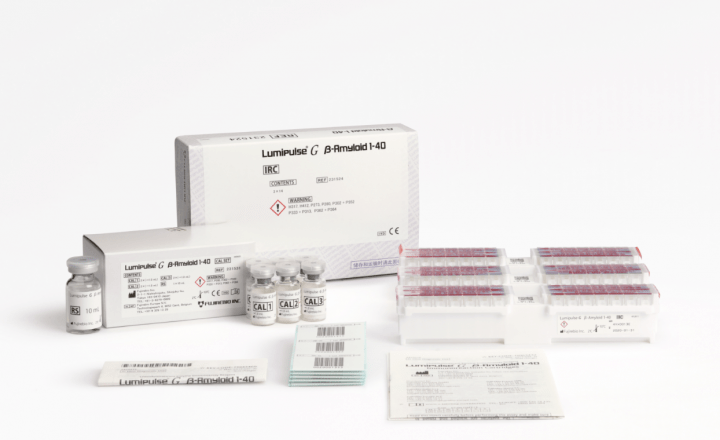
Another study by Bannon et al.2 (LB14 – Evidence that Lumipulse G pTau217 Plasma measurements have the ability to quantitatively assess Tau stage and burden – S44-45) focused on the utility of blood-based biomarkers in predicting both amyloid positivity as measured with amyloid PET as well as tau burden as measured with tau PET. The plasma Aβ1-42/Aβ1-40 ratio and plasma pTau217 were determined in samples from 387 participants in the Australian Imaging, Biomarker & Lifestyle Flagship Study of Aging (AIBL). The study population included individuals along the AD continuum from cognitively normal individuals over MCI to AD and non-dementia patients, having both types of imaging available. While both biomarkers show significant differences between the amyloid positive and negative individuals within each clinical group, plasma pTau217 outperforms the plasma Aβ1-42/Aβ1-40 ratio (AUC 0.93 vs. 0.84, respectively) in predicting amyloid PET positivity. In addition to this, plasma pTau217 strongly correlates with tau burden and the receiving operator characteristics (ROC) curve analysis using the medial temporal lobe tau burden and the overall Braak staging results both in an AUC of 0.93. These results suggest that plasma pTau217 can be seen as a marker for amyloid as well as tau pathology and has the potential to distinguish between low and intermediate/high AD neuropathological change, especially for tau.
Taken together, the evidence for the potential of blood-based biomarkers is accumulating, and in combination with the pending availability of disease-modifying treatments there is good reason for the AD field to be optimistic. However, key elements to consider before implementation are, among others, the context of use with its associated prior probability of amyloid/tau pathology, the testing paradigm and whether that includes confirmation by CSF and/or PET, the impact of the same pre-analytical factors studied in much detail for CSF biomarkers, the effect of co-morbidities that are often numerous in an elderly population, education of health care professionals regarding the interpretation, advantages and limitations of the use of plasma biomarkers, and many more.
References:
- Revised Criteria for Diagnosis and Staging of Alzheimer's | AAIC
- CTAD ABSTRACT 2023 oct 24_compressed.pdf (ctad-alzheimer.com)
- Janelidze et al., JAMA Neurol 2021 Nov 1;78(11):1375-1382.
- Pannee et al., Alzheimers Dement (Amst) 2021; Oct 14;13(1):e12242.
- Zicha et al., Alzheimers Dement 2022; Jul 12:10.1002/alz.12697.
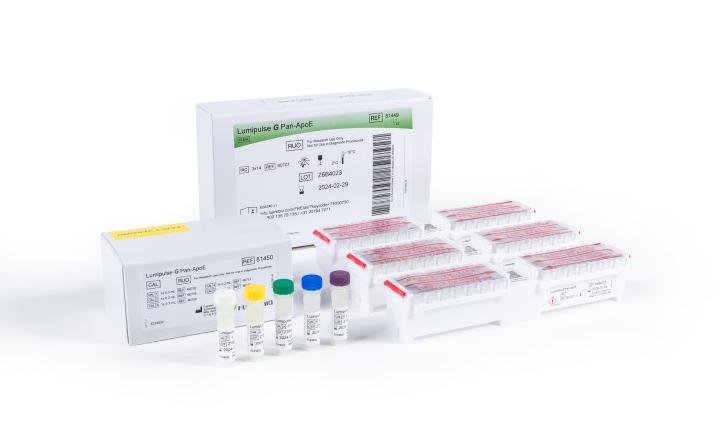
Note: The Lumipulse G β-Amyloid 1-42 Plasma, Lumipulse G β-Amyloid 1-40 Plasma, Lumipulse G pTau 181 Plasma and Lumipulse G pTau 217 Plasma assays referred to in the abovementioned publications are Research Use Only or prototype version thereof (in the case of Lumipulse G pTau 217 Plasma), and therefore not for use in diagnostic procedures.