Comparison of Aβ1-42/Aβ1-40 ratio with other ratios
Previous posts in this series:
- Use of the Aβ1-42/Aβ1-40 ratio to improve accuracy of AD diagnosis
- Aβ1-42/Aβ1-40 ratio for interpretation of discordant results
- Improvement of AD risk scores by use of the Aβ1-42/Aβ1-40 ratio
- How to work with Aβ1-42/Aβ1-40 ratio
Don't miss the upcoming related Insight articles over the next weeks and get deeper information on the value of using Aβ1-42/Aβ1-40 ratio. Or simply download the complete guidance document now! (requires a Premium eServices account)
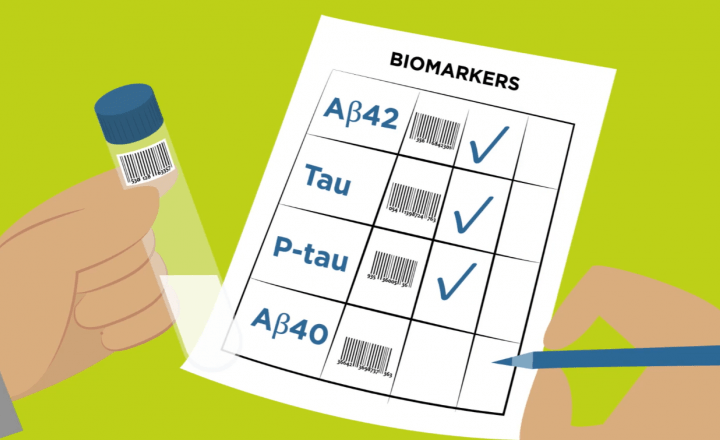
- Combinations of different biomarkers outperform the use of individual biomarkers alone.
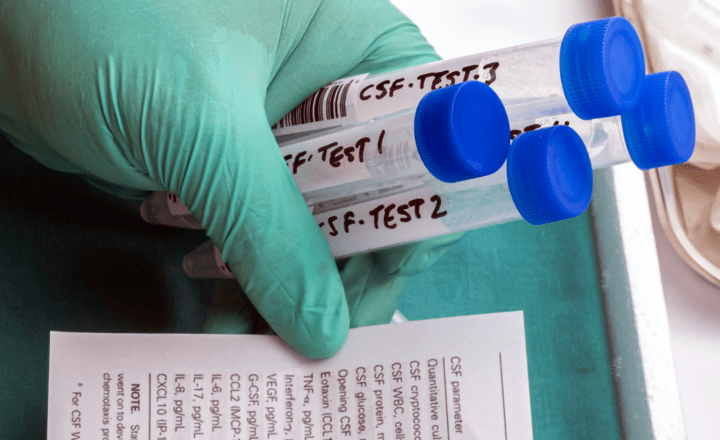
- Several biomarker combinations have been tested and used in different kinds of ratios for AD diagnostics (t-Tau/Aβ1-42 ratio, p-Tau/Aβ1-42 ratio, Aβ1-42/Aβ1-38 ratio) with good sensitivity and specificity.
- However, combining different physiopathologies (e.g. Tau and amyloid), the ratios must be used in a very strict context, according to a well-defined clinical question.
- CSF Aβ1-42/Aβ1-40 can be used as a tool to normalize values of amyloid levels, other ratios might be seen more as interpretation tools.
CSF Aβ1-42/Aβ1-40 is a tool to normalize values of patients with different amyloid levels, as other ratios might be seen more as interpretation tools which allow to compare different biomarker results.
Whereas other ratios combine different pathological features, the Aβ1-42/Aβ1-40 ratio is a combination of two markers reflecting the same pathology. As soon as other biomarkers such as tTau or pTau are included, it must be taken into consideration that Tau and Aβ might not have a linear relationship all over the course of the disease as they are parts of different pathological pathways. Therefore, every use of a ratio combining different pathologies needs to be evaluated and assessed very critical with regard to its value and result at different states of the disease and lifespan of the patient.
Tau / amyloid ratios
Among the scientific community it is generally widely accepted that combinations of different biomarkers outperform the use of individual biomarkers alone. The ongoing discussions are more related to the question about the best combination to predict or differentially diagnose AD.
Based on the sensitivity of the best performing regression formulas, Duits et al. (2015) recommend the use of a tTau/Aβ1-42 ratio, as the use of this combination constitutes a robust CSF AD Alzheimer profile. They also evaluated pTau/Aβ1-42 ratio, which was found to predict AD with a sensitivity of 91%–93%, and a specificity of 81%–84%. The same combinations (tTau/Aβ1-42 and pTau/Aβ1-42) best predicted cognitive decline in mild cognitive impairment patients. Validation confirmed these results, especially regarding the tTau/Aβ1-42 ratio.4
The Alzheimer Disease Neuroimaging Initiative (ADNI), an international consortium, has been a key cohort study for predicting the progression from MCI to AD using biomarkers, and demonstrated that the tTau/Aβ1-42 ratio could be used to predict conversion from MCI to AD dementia, revealing a sensitivity of 86% and specificity of 85%.1;2
Nevertheless, since there are other pathologies (e.g. Tau), and other ratios that can combine different pathological models to evaluate the AD risk, all ratios must be used in strict context, according to a well-defined clinical question.
Other amyloid / amyloid ratios
It seems that between Aβ1-42/Aβ1-40 ratio and Aβ1-42/Aβ1-38 ratio there is not much difference. Aβ1-38 may be increased in neuroinflammatory diseases.3 But since the assays for Aβ1-40 are well-established, which is not the case for Aβ1-38, and in addition there is not enough data on Aβ1-38, Aβ1-42/Aβ1-40 ratio seems to be the better option in this comparison.
References
- Petersen, R. C., et al. "Alzheimer's disease neuroimaging initiative (ADNI): clinical characterization." Neurology 74.3 (2010): 201-209.
- Ritchie, Craig, et al. "CSF tau and the CSF tau/ABeta ratio for the diagnosis of Alzheimer's disease dementia and other dementias in people with mild cognitive impairment (MCI)." Cochrane Database of Systematic Reviews 3 (2017).
- Wiltfang, Jens, et al. "Highly conserved and disease‐specific patterns of carboxyterminally truncated Aβ peptides 1–37/38/39 in addition to 1–40/42 in Alzheimer's disease and in patients with chronic neuroinflammation." Journal of neurochemistry 81.3 (2002): 481-496.
- Duits, Flora H., et al. "The cerebrospinal fluid “Alzheimer profile”: easily said, but what does it mean?" Alzheimer's & Dementia 10.6 (2014): 713-723.
Don't miss the next posts on this topic in the following weeks:
Related articles
Video - Alzheimer's awareness redefined
Follow the journey of the Sullivan family and leading Alzheimer’s Neurologist and Researcher Dr. David Greeley as they introduce and explain these...
Publication - Serum and cerebrospinal fluid neurofilament light chains measured by SIMOA™, Ella™, and Lumipulse™ in multiple sclerosis naïve patients
We would like to draw your attention to a first publication on our Lumipulse® G NfL solution. In this article you will find a method comparison of CSF...
CTAD 2023 – Spotlight on recent advances in blood-based biomarkers for Alzheimer’s disease
Both fluid and imaging biomarkers provide biological evidence for the underlying etiology of cognitive impairment. The core fluid biomarkers of...
IVDR status update for Fujirebio’s Neuro products
The European CE-marking is used to support registrations of in vitro diagnostic (IVD) medical devices in many jurisdictions around the world. The...
Scientific poster - Blood sample matrix validation, impact of sample freezing and method comparison analysis using the Lumipulse® G NfL blood prototype assay
This AD/PD 2023 poster investigates the agreement between matched serum and plasma samples on the Lumipulse G NfL Blood prototype assay, the impact of...
Video - A neurochemist's search to save memories
Meet Dr. Charlotte Teunissen, Professor in Neurochemistry, and her lifelong friend Christa Reinhoudt, who was diagnosed with Alzheimer's disease in...
Scientific poster - Analytical performance of the Lumipulse® G NfL CSF <RUO>
Poster presented at the AD/PD 2023
This AD/PD 2023 poster wishes to demonstrate the analytical performance of the newly developed Lumipulse G NfL CSF...
Scientific poster - A fully automated and scalable plasma pTau181 assay for Alzheimer's disease
In this article, the diagnostic performance of a modified version of the Lumipulse G pTau181 CSF test is evaluated.
Scientific poster - CSF pTau181/Aβ1-42 ratio increases pre-analytical variability over measuring Aβ1-42 alone
In this CTAD 2022 poster, we examine the utility of CSF biomarker ratios to correct for pre-analytical variability.
New criteria for Alzheimer’s disease
New criteria for different stages of AD have been suggested by the International Working Group (IWG) and the National Institute on Aging-Alzheimer’s...
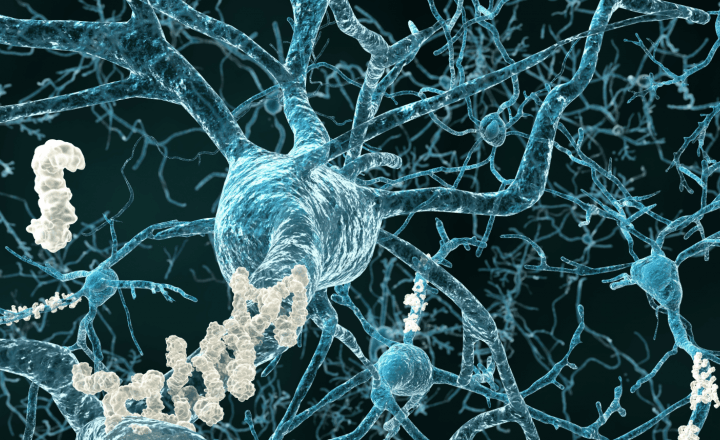
Aβ deposition and clearance: a key feature of the ageing brain
This chapter looks closer at Aβ deposition and clearance as key feature of ageing brain.
Scientific poster - Analytical performance of the Lumipulse® G β-Amyloid 1-40 Plasma and Lumipulse® G β-Amyloid 1-42 Plasma RUO assays
The aim of the study, presented at the AAIC 2022, was to determine the performance of several analytical parameters, including amongst others...
Scientific poster - Reducing misdiagnosis of Alzheimer’s disease pathology utilizing CSF and amyloid PET
In this poster we examine the performance of cognitive testing alone for identification of amyloid positivity in MCI patients from the ADNI study when...
Scientific poster - Analytical performance overview of the Lumipulse® G pTau 181 Plasma RUO assay
The aim of the study, presented at the AAIC 2022, was to determine the performance of several analytical parameters, including amongst others...
CSF biochemical pattern interpretation
What are some of the best-practices of CSF biochemical pattern interpretation? In this article series we aim at highlighting the current state of...
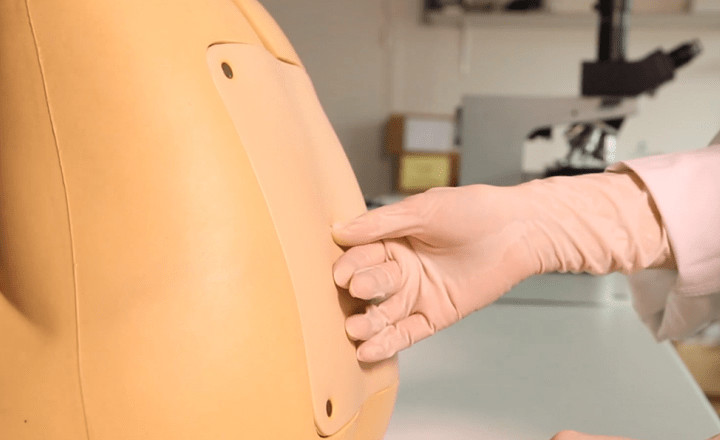
Handling and transportation of CSF samples
Cerebrospinal fluid (CSF) can be collected in the lumbar region by an experienced physician. This article details the recommended procedure for...
How to perform a lumbar puncture
In this article series we aim at highlighting the current state of knowledge and the latest developments in the field of Alzheimer’s disease (AD)...
Using CSF biomarkers to link pathology and clinical presentation
In this article series we aim at highlighting the current state of knowledge and the latest developments in the field of Alzheimer’s disease (AD)...
Video - A day at the Fujirebio Neuro Center of Excellence
In this short video we show you around at the Fujirebio Neuro Center of Excellence. Right now, expectations are high for the development of blood...
Altered proteins in brain neurodegenerative diseases
In this new article series we aim at highlighting the current state of knowledge and the latest developments in the field of Alzheimer’s disease (AD)...
Scientific poster - Comparing CSF and plasma LUMIPULSE® Alzheimer’s Disease biomarker analysis to amyloid-β PET imaging
The aim of this study was to evaluate a plasma pTau biomarker as a tool for predicting amyloid pathology.
Improving clinical diagnosis of Alzheimer’s disease: Review of the available literature
In this chapter, we will review available literature on the accuracy of the underlying pathological determinations in mild cognitive impairment (MCI)...
The drawbacks of relying solely on the standard routine clinical examinations and cognitive testing
Many subtypes of disease exist under the umbrella of dementia with Alzheimer’s disease (AD) being the most common. AD-related dementia is...
Testimonial - Value of the β-Amyloid ratio and other CSF biomarkers in the Erlangen Score interpretation algorithm
By Prof. Dr. Piotr Lewczuk - Two groups of established cerebrospinal fluid (CSF) biomarkers reflect two major pathological alterations in Alzheimer's...
Webinar replay - Possible applications for novel CSF biomarkers
At Fujirebio we have been hosting a webinar series with leading expert speakers dedicated to current topics in the field of Alzheimer's disease...
Webinar series - Current topics in Alzheimer's disease diagnostics
We have been hosting a series of 3 webinars with leading expert speakers and dedicated to current topics in the field of Alzheimer's Disease...
Scientific poster - Towards an easy plasma pTau 181 detection
Blood-based Alzheimer’s disease (AD) biomarker testing could be used as a simple, accessible, and scalable approach to help support the diagnosis of...
Video - The interest of automated testing for all four CSF biomarkers
In less than 2 minutes, this video explains the advantages of automated biomarker testing for all four CSF biomarkers, over other available testing...
Webinar replay - Preparing for the future of plasma based Alzheimers disease diagnostics
At Fujirebio we are hosting a webinar series with leading expert speakers dedicated to current topics in the field of Alzheimer's disease diagnostics...
Webinar replay - CSF-based biomarkers to support the diagnosis of Alzheimer’s disease
At Fujirebio we are hosting a webinar series with leading expert speakers dedicated to current topics in the field of Alzheimer's disease diagnostics...
The Fujirebio Neuro Center of Excellence
The Fujirebio Neuro Center of Excellence has been founded with the objective of rising to this challenge. It is a research and development hub focused...
Booklet - First edition of our new clinical booklet "A few drops of insight can lead to an ocean of understanding"
Early diagnosis of Alzheimer's disease is crucial. The desire to tackle neurodegenerative diseases by always finding earlier diagnostic solutions and...
Video - Ratio calculation of Aβ1-42 and Aβ1-40 offers essential information about the buildup of amyloid pathology in a patient's brain
This 2 minute video explains why and how a ratio calculation of the two amyloid proteins, Aβ1-42 and Aβ1-40, offers particularly essential information...
Video - Daniel's story about his early testing and diagnosis of Alzheimers disease
Daniel lives in Stockholm, Sweden, and was diagnosed with Alzheimer’s disease when he was still in his early 50's. In this 6-minute video we follow...
Influence of automation on Aβ1-42/Aβ1-40 ratio and its use
Automation is an important step in the direction of more standardization as it limits the number of manual handling steps and therefore minimizes...
How to work with Aβ1-42/Aβ1-40 ratio
One cause of discordant results can be the preanalytical conditions, e.g. when laboratories use tubes that bind certain proteins. Aβ1-42 adsorption is...
Improvement of AD risk scores by use of the Aβ1-42/Aβ1-40 ratio
Different scores have been developed to provide an interpretation of biomarker results for AD diagnosis or risk prediction. Here we will give two...
Aβ1-42/Aβ1-40 ratio for interpretation of discordant results
By use of the Aβ1-42/Aβ1-40 ratio, discordant results (i.e. when amyloid and tau biomarkers are not concordant) can be improved. However, while the...
Use of the Aβ1-42/Aβ1-40 ratio to improve accuracy of AD diagnosis
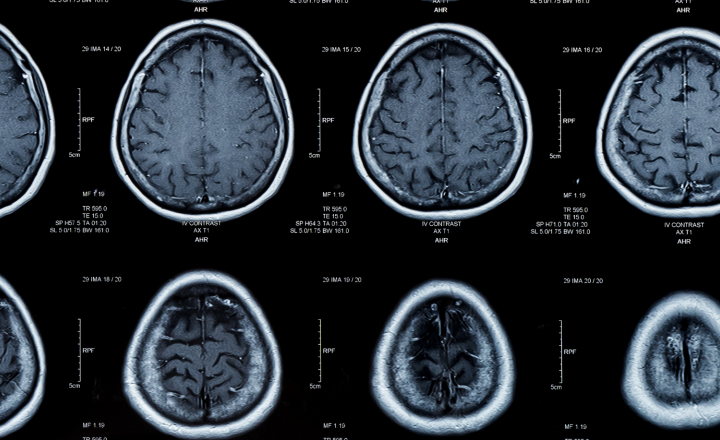
It is widely agreed that, since cerebrospinal fluid (CSF) is in direct contact with the central nervous system (CNS), analytes measured in this body...
What is Alzheimer's disease?
Alzheimer’s disease, which is the most common form of dementia, is an incurable degenerative disease. Neurons in certain parts of the brain are...