EUROGIN 2024 – key takeaway messages
By Rebecca Millecamps, Fujirebio
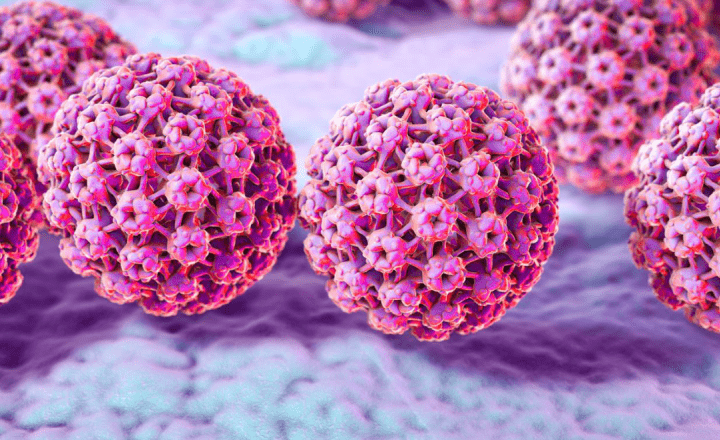
The annual EUROGIN conference covers a dense scientific program on the topic of Human papillomavirus (HPV) and its associated cancers, always with a strong focus on the patient. This year’s edition in Stockholm, Sweden was no exception. Bringing together attendees from all over the world, EUROGIN 2024 offered a global perspective on the current challenges and successes in prevention, diagnosis and treatment of high-grade precancerous lesions, cervical cancer, and other HPV-related diseases. In this article we review what we see as the key takeaway messages of the conference.
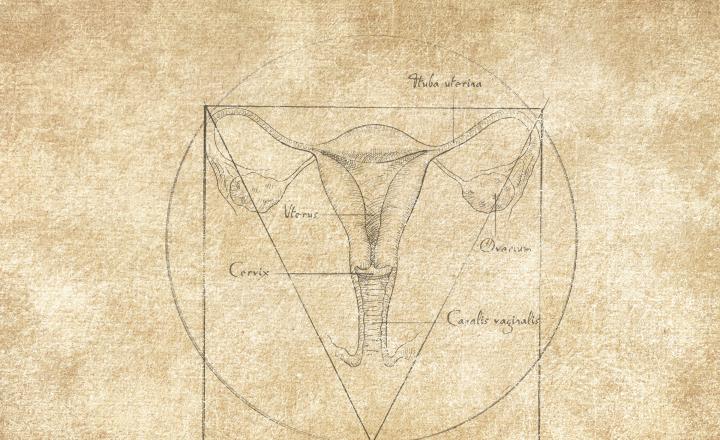
Towards more effective and efficient cervical cancer screening in Europe
The burden and control of cervical cancer is changing a lot. About 70 percent of the European population has access to an organized screening program, however cervical cancer is still common. Screening would be more effective and efficient by directing screening resource to those most at risk. Most screening programs today report unnecessary colposcopy referrals of about 80 to 90 percent. Risk-based screening will be increasingly important in a future mixed population of highly vaccinated young people and older non-vaccinated population, with high variance in cancer risk. The implementation of a risk-based cervical cancer screening is being evaluated and a European consortium, the Risk-based Screening for Cervical Cancer (RISCC), aims to develop and implement risk-based HPV screening strategies.
Cervical cancer screening programmes are evolving rapidly with the introduction of new technologies and with the arrival of vaccinated women in screening programs. What will be the role of cytology in the coming years? It has already changed from primary screening test to triage test to increase the specificity of HPV testing. The HPV screening protocols are evolving further towards molecular testing to detect those at high risk of progression.
With the implementation of self-collected samples, the increased use of HPV genotyping and interest in point-of-care tests, more extended principles and concepts are needed for the validation of HPV tests for primary screening. HPV-type specific performance, ranking of HPV genotypes, impact of storage/transport media or collection methods and devices used, are all topics of concern and are widely debated as is also reflected in the EUROGIN program.
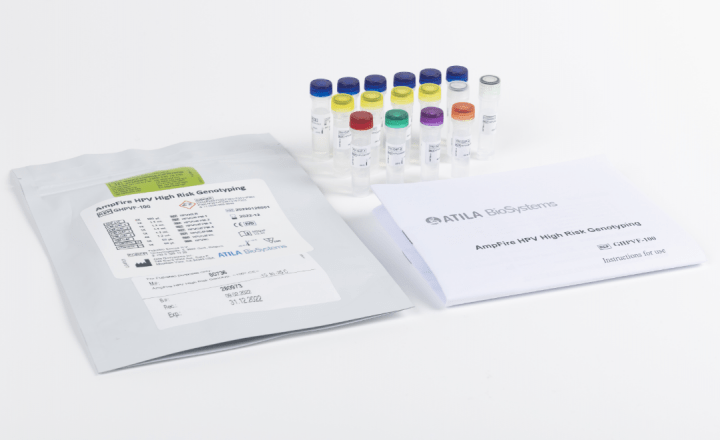
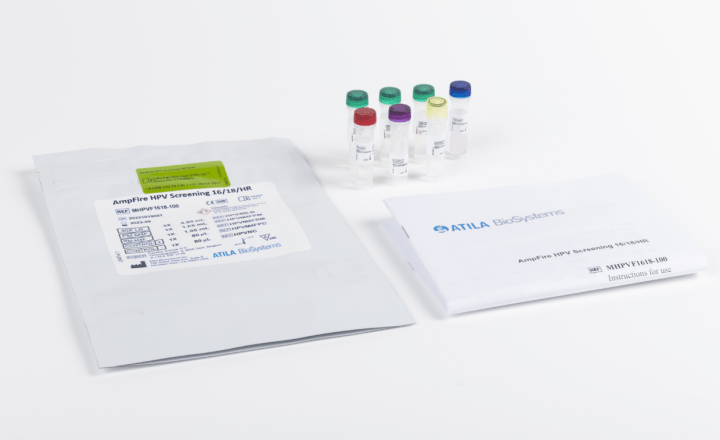
HPV genotyping – a tool for triage and patient management
As each high-risk HPV (hrHPV) genotype carries a different risk of progression to cervical cancer, HPV genotyping can be used to manage HPV-positive women accordingly. The use of HPV genotyping for triage and management is gaining importance worldwide. HPV16/18 positivity is currently being included in several clinical algorithms to support the direct referral to colposcopy. The inclusion of extended genotyping and further identification of the other hrHPV genotypes, is being piloted to further stratify patient risk and guide their management.
Questions arise on whether HPV screening tests need to be redesigned to include other or less HPV genotypes. Making these decisions will be quite challenging and will take several years, and input from epidemiology studies will be needed.
Methylation analysis – an added value for improved risk stratification and patient management
DNA methylation has evolved as one of the most promising tools for the early detection of HPV-associated cancer. Large clinical studies have demonstrated the applicability of DNA methylation analysis as triage method in HPV-based cervical screening. Methylation assays are now commercially available and although they are not in the screening guidelines yet, the use of methylation markers for detection of HPV-induced cancers, including anogenital and oropharyngeal cancers is widely being evaluated. Studies of methylation testing show promising diagnostic and prognostic value in cervical cancer screening and treatment of cervical, vulvar, and anal intraepithelial neoplasia.
Methylation is clearly of interest for triage of HPV positive women, as the lack of trained cytologists will be a persistent problem. Because of its applicability on self-collected samples, methylation offers the possibility of a full molecular workflow and a high-quality screening with limited loss of follow-up. Different scenarios for a full molecular workflow are investigated, for example adding methylation analysis to HPV genotyping based screening.
Self-sampling – a key for improved cervical cancer screening
Self-collection-based screening programs aim to reduce inequities in access to screening. Based on current available data, HPV testing done with clinically validated PCR-based assays has similar performance on self-collected and clinician-collected samples in terms of detection of high-grade cervical epithelial lesions (CIN2+ or CIN3+).
Several real-world examples have shown the feasibility of self-sampling for HPV primary screening. In the Netherlands, Denmark, Sweden and Australia, self-sampling has been implemented and today it represents a significant portion of participation rate ranging from 27% in Australia to 50% in the Netherlands. In Denmark, there was a 30% screening uptake after dedicated invitation for self-sampling to women who did not participate initially. HPV testing on self-collected samples has been identified as a cost-effective strategy when it yields population coverage gain.
Further considerations on quality of HPV self-sampling include but are not limited to: validation of combination of HPV test and self-sampling device, impact of sample dilution and pre-analytical sample processing, monitoring of invalids, … These considerations related to self-sampling are also being discussed for future updates of the clinical validation guidelines for cervical cancer screening.
HPV prevalence and genotype distribution
Today, epidemiological studies are essential to monitor the progress in global prevention and to reveal new characteristics of the natural history of HPV infection. These insights can lead to improved effectiveness of HPV vaccination and early detection and prevention of not only cervical cancer but also other HPV-associated cancers, such as anal cancer, vulvar cancer, and oropharyngeal cancer.
Full HPV genotyping is important to get insights into the global burden of cervical HPV infections, time trends in HPV prevalence and genotype distribution in HPV-associated cancers, prevalence of HPV at different steps of assisted reproduction technology procedures, changes in the disease burden of HPV-related cancers, etc.
Surveillance of what happens post-HPV vaccination is warranted. The effectiveness of HPV screening programs in unvaccinated and vaccinated cohorts, and the role of new technologies in future screening are evaluated. Evaluation of the risk of precancer in vaccinated cohorts showed the unmasking of other HPV-genotypes such as HPV33 when HPV16 disappears in the vaccinated population. Risk of precancer by genotyping result and HPV replacement needs to be carefully analysed because the risks and test performance are changing over time as the HPV prevalence is also changing. The attributable fraction of HPV genotypes detectable in high-grade lesions will be affected by vaccination. In Scotland, for example, HPV82 enters the top 5 of HPV genotypes related to high grade disease. The relative contribution in CIN2 and CIN3 of non-HR was respectively 4.9% and 1.6% in unvaccinated cases while representing 13% and 7.8% in vaccinated cohort. It is plausible that the properties and carcinogenic progression rate of pre-invasive lesions, particularly CIN2, will change in vaccinated women.
Definitely never a dull moment when it comes to HPV, screening, diagnosis, and treatment of HPV-associated diseases.
It’s all about transforming scientific insights into public health policies and practice in the field, enabling clinicians to integrate the basic and advanced principles in diagnosis and management of cervical-vaginal, vulvar, and anal diseases in their everyday practice.
Ultimately contributing to improved patient outcomes.