A risk-based approach for post-treatment detection of recurrent CIN
By Rebecca Millecamps, Fujirebio
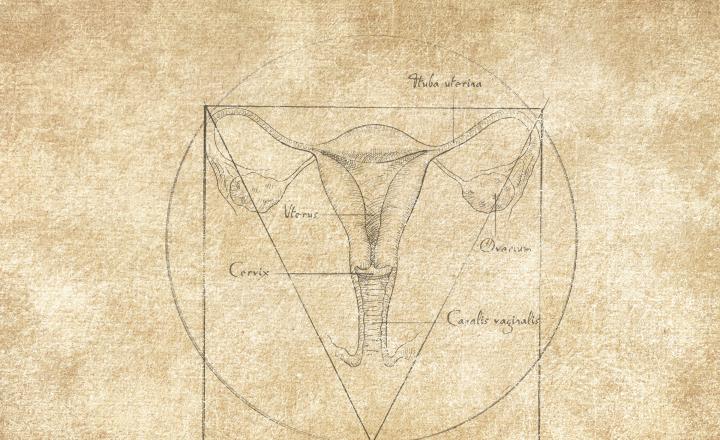
Women who are treated for CIN2/3 remain at increased risk of recurrent CIN and cervical cancer. Therefore, strategies to monitor these women after treatment are implemented in many countries. The most common posttreatment surveillance method to detect recurrent CIN include HPV testing and/or cytology. Methylation markers are promising tools for reliable posttreatment detection of recurrent CIN2/3 with a persistent HPV infection following treatment of high-grade CIN. Unnecessary interventions should be avoided, since (re)treatment of CIN is associated with an increased risk of obstetric complications.
This article describes how HPV genotyping and DNA methylation analysis can help discriminate women in need of re-treatment from those who can be managed conservatively to prevent overtreatment.
The article is part of a series of resources dedicated to the state-of-the-art of HPV testing.
Get a full overview of our resources here.
Treatment of high-grade cervical intraepithelial neoplasia (CIN2/3) is effective in preventing subsequent invasive cervical cancer, but despite treatment these women remain at increased risk of developing a new CIN for the next 25 years compared to the general population. The majority of cases develop within the first two years after treatment and approximately 7% of treated women are diagnosed with recurrent disease during the 18-month follow-up period. In view of the substantial risk of recurrent disease, effective post-treatment testing is mandatory.1,2,3,4,5,6
Careful clinical surveillance is a necessary condition for effectiveness of conservative treatments of cervical intraepithelial neoplasia (CIN) from both a clinical and a public health perspective. The rate of patients lost to follow-up is often not documented, although figures as high as 25% have occasionally been observed.7
Recurrent cervical high-grade lesions – a heterogenous group
Recurrent cervical high-grade lesions represent a heterogenous group, including either persisting lesions resulting from incomplete treatment (residual lesions) or newly develop lesions (incident lesions). Most of the recurrent high-grade lesions diagnosed within two years of surgery are actually residual lesions. Several factors influence the recurrence of high-grade lesions. For example, a persistent HPV16 infection is associated with a greater rate of relapse after conisation of CIN2+ with respect to the other high risk HPV genotypes.13,14
Persistent versus new HPV infection
The strong etiological link between persistent high-risk HPV-infection and the development of cervical cancer is clear. A new infection of a different HPV genotype gives a relatively low future risk, given the probability of clearance of the infection and the long interval after HPV infection before the development of an invasive cancer. A negative high-risk HPV result has a superior negative predictive value (NPV) compared with negative cytology or negative resection margins. Posttreatment negative co-testing avoids an additional 8.4 cases of CIN3 or worse per 1,000 women treated and reduce health care costs, compared with negative cytology alone.12
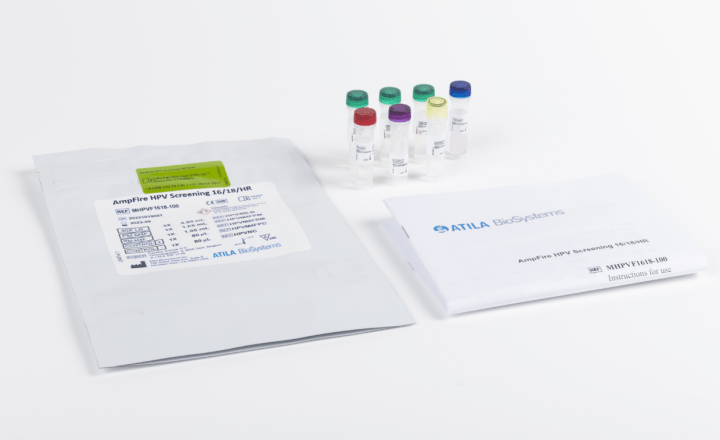
Incorporating HPV testing post-treatment shown to be safe and cost effective
hrHPV-testing, cytology or both (co-testing) have been evaluated for prediction of post-treatment disease. Co-testing gives the best results in terms of sensitivity but at the expense of lower specificity. Today, guidelines for follow-up after treatment of CIN2/3 recommend co-testing at 4-6, 12 and 24 months.8,9,10,11 For example, in Canadian context, strategies that incorporate HPV testing post-treatment have been shown to be safe and cost effective by reducing subsequent colposcopy visits and repeat treatments without impacting cervical cancer incidence and mortality rates.8
The Australian guidelines for test of cure following treatment for high-grade squamous abnormalities already include partial genotyping (individual reporting of HPV16 and HPV18 and the remaining group of other 12 high-risk HPV).9
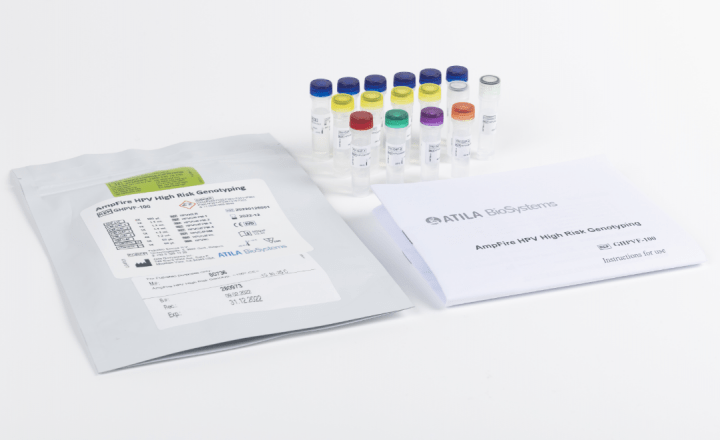
A clear benefit by adding HPV genotyping in pre-and post-treatment testing
To individualize the posttreatment surveillance, better identification of women with relevant HPV genotype presence may be a benefit. Reporting a genotype that was present before the treatment permits the distinction between same-genotype persistence and a new infection. It is demonstrated that qualitative pooled HPV results have a good clinical utility for posttreatment follow-up. However, studies also reported that new HPV infections (with clearance of the pre-treatment genotype) accounted for a median of 60% of positive posttreatment HPV results. The risk of CIN2 or worse after treatment is very low in the case of a new HPV infection. In case of persistence with the same HPV genotype, the risk of CIN2 or worse after treatment was much higher. There is clearly a benefit by adding HPV genotyping in pre- and post-treatment testing, making it possible to distinguish women post-treatment with a need for repeat colposcopy, biopsy and consideration of repeat treatment from those women with a recommendation for a more conservative follow-up with retesting.12
Information on the frequency of newly detected HPV genotypes following treatment for cervical precancer and cancer may also aid in determining whether vaccination has a benefit in treated women.13
New biomarkers have shown already promise for improved detection of precancers
Next to HPV/cytology co-testing, the performance of several other markers for the monitoring of women treated for high grade CIN is being explored and show promise for improved detection of precancers.
Residual and newly developed CIN look morphologically similar. Today, all recurrent lesions are treated similarly to prevent progression to cervical cancer. However, the short-term risk of progression to cervical cancer of residual and newly developed lesions might be different. Newly developed lesions probably have a lower short-term risk of progression to cancer compared with residual lesions, and therefore these lesions may not need immediate treatment. In addition, CIN lesions can show spontaneous regression in 40% to 50% of CIN2 and 30% of CIN3.
Treatment of CIN is associated with an increased risk of obstetric complications, therefore unnecessary interventions should be avoided.
DNA methylation of human genes has shown to be particularly sensitive for the detection of cervical cancer and advanced CIN2/3, that is, lesions caused by a long-lasting persistent high-risk HPV infection with a presumed increased short-term risk of progression to cervical cancer. Absence of host-cell DNA methylation, on the other hand, is associated with regression of CIN2/3.
Posttreatment monitoring by methylation analysis of ASCL1/LHX8 and FAM19A4/miR124-2 showed a good performance for the detection of recurrent CIN. DNA methylation testing could therefore be an interesting strategy to detect recurrent CIN after treatment, in particular for the detection of residual lesions in need of re-treatment.14
References
- M.R.E. McCredie et al. Natural history of cervical neoplasia and risk of invasive cancer in women with cervical intraepithelial neoplasia 3: a retrospective cohort study. Lancet Oncol (2008). Natural history of cervical neoplasia and risk of invasive cancer in women with cervical intraepithelial neoplasia 3: a retrospective cohort study - The Lancet Oncology
- Kocken M. et al. Risk of recurrent highgrade cervical intraepithelial neoplasia after successful treatment: a long-term multi-cohort study. Lancet Oncol. 2011;12(5):441-450. Risk of recurrent high-grade cervical intraepithelial neoplasia after successful treatment: a long-term multi-cohort study - The Lancet Oncology
- Rebolj M. et al. Risk of cervical cancer after completed post-treatment follow-up of cervical intraepithelial neoplasia: population based cohort study. BMJ. 2012;345:e6855. doi: https://doi.org/10.1136/bmj.e6855
- Soutter WP et al. Long-term risk of invasive cervical cancer after treatment of squamous cervical intraepithelial neoplasia. Int J Cancer. 2006;118(8):2048-2055. Long‐term risk of invasive cervical cancer after treatment of squamous cervical intraepithelial neoplasia - Soutter - 2006 - International Journal of Cancer - Wiley Online Library
- Kalliala I. et al. Incidence and mortality from cervical cancer and other malignancies after treatment of cervical intraepithelial neoplasia: A systematic review and meta-analysis of the literature. Ann. Oncol. 2020;31:213–227. Incidence and mortality from cervical cancer and other malignancies after treatment of cervical intraepithelial neoplasia: a systematic review and meta-analysis of the literature - Annals of Oncology
- Arbyn M. et al. Incomplete excision of cervical precancer as a predictor of treatment failure: A systematic review and meta-analysis. Lancet Oncol. 2017;18:1665–1679. content (helsinki.fi)
- Cristiani P. et al. Follow-up of screening patients conservatively treated for cervical intraepithelial neoplasia grade 2–3, Eur J Obstet Gynecol Reprod Biol. 2007 Aug;133(2):227-31.
- Willows K. et al. 2023 Canadian colposcopy guideline: a risk-based approach to management and surveillance of cervical dysplasia. Curr. Oncol. 203, 30, 5738-5768. Current Oncology | Free Full-Text | 2023 Canadian Colposcopy Guideline: A Risk-Based Approach to Management and Surveillance of Cervical Dysplasia (mdpi.com)
- Clinical guidelines Cancer Council Australia.
- Perkins R.B. et al. 2019 ASCCP Risk-Based Management Consensus Guidelines for Abnormal Cervical Cancer Screening Tests and Cancer Precursors. J. Low. Genit. Tract Dis. 2020;24:102–131. 2019 ASCCP Risk-Based Management Consensus Guidelines for Abnormal Cervical Cancer Screening Tests and Cancer Precursors - PMC (nih.gov)
- Jordan J. et al. European guidelines for clinical management of abnormal cervical cytology, Part 2. Cytopathology. 2009;20:5–16. Eu-guidelines-part-2.pdf (efcolposcopy.eu)
- Bottari F. et al. Human Papillomavirus Genotyping Compared With a Qualitative High-Risk Human Papillomavirus Test After Treatment of High-Grade Cervical Intraepithelial Neoplasia: A Systematic Review. Obstetrics & Gynecology 134(3):p 452-462, September 2019. Human Papillomavirus Genotyping Compared With a Qualitative High-Risk Human Papillomavirus Test After Treatment of High-Grade Cervical Intraepithelial Neoplasia - PMC (nih.gov)
- Rositch AF et al. The incidence of human papillomavirus infection following treatment for cervical neoplasia: a systematic review. Gynecol Oncol. 2014 Mar;132(3):767-79. The incidence of human papillomavirus infection following treatment for cervical neoplasia: A systematic review - PMC (nih.gov)
- Dick S. et al. Methylation testing for the detection of recurrent cervical intraepithelial neoplasia. Int J Cancer. 2023;1‐8. Methylation testing for the detection of recurrent cervical intraepithelial neoplasia - Dick - International Journal of Cancer - Wiley Online Library